Department of Surgery Women's Council

The University of Washington Department of Surgery Women’s Council originated in 2016 with the mission to promote gender equity in surgery. Women’s council initially included members from all practice sites and divisions and was comprised of both faculty and resident members. The council was divided into a faculty and resident council in 2018 to better address the unique issues that impact women at different career levels. A Women’s Council sponsored Association of Women Surgeons UW School of Medicine Student chapter was added in 2019 to foster development of medical students interested in entering a surgical field. Although specifically developed to advise Dr Wood on issues impacting women faculty and trainees within the department, the overarching goal of the council is to improve the working environment for all.
The faculty women’s council has been in existence since 2016 and current members range from assistant to full professors. The University of Washington (UW) Department of Surgery (DOS) Faculty Women's Council empowers and supports faculty with the goal of promoting gender equity in surgery.
One of the first tasks undertaken by the council was a survey to better understand if gender was perceived as a barrier to a surgical career within our own department at either the faculty or resident level. A department wide career barriers survey was administered and results presented at the inaugural annual Women’s Council Grand Rounds in February 2018 by Drs. Kris Calhoun, Sherene Shalhub and Nicole Zern. It was ultimately presented as a podium presentation at the Pacific Coast Surgical Association annual meeting in 2019 and published in JAMA Surgery.
Inaugural Annual Women’s Council Grand Rounds - February 2018

Top row: Sarah Atkinson (Assistant Professor, General Surgery/UW Medicine-Montlake), Kathleen Berfield (Associate Professor, Cardiothoracic/Thoracic), Erika Bisgaard (Assistant Professor, Trauma/Harborview Medical Center), Eileen Bulger (Professor, General Surgery/Harborview Medical Center) (Advisory member), Kris Calhoun, Chair (Professor, General Surgery/UW Medicine-Montlake), Judy Chen (Assistant Professor, General Surgery/UW Medicine-Montlake)
Second row: Shannon Colohan (Associate Professor, Plastics/UW Medicine-Montlake), Kirsten Dansey (Assistant Professor, Vascular/UW Medicine-Montlake), Meghan Flanagan (Assistant Professor, General Surgery/UW Medicine-Northwest), Sarah Greenberg (Assistant Professor, Pediatric Surgery/Seattle Children’s Hospital), Sarah Goldsberry-Long (Assistant Professor, Plastics/UW Medicine-Montlake), Sara Javid (Professor, General Surgery/UW Medicine-Montlake) (Advisory member)
Third row: Teresa Kim (Assistant Professor, General Surgery/UW Medicine-Montlake), Catherine Kling (Assistant Professor, Transplant/UW Medicine-Montlake), Lorrie Langdale (Professor, General Surgery/VA Puget Sound Health Care System), Rachel Lentz (Assistant Professor, Plastics/UW Medicine-Montlake), Deb Marquardt (Assistant Professor, General Surgery/VA Puget Sound Health Care System), Emily Palmquist (Assistant Professor, General Surgery/UW Medicine-Northwest)
Fourth row: Zoe Parr (Clinical Associate Professor, GS/UW Medicine-Northwest), Rebecca Petersen (Associate Professor, General Surgery/UW Medicine-Northwest), Lena Sibulesky (Associate Professor, Transplant/UW Medicine-Montlake), Caitlin Smith (Assistant Professor, Pediatrics/Seattle Children’s Hospital), Sara Zettervall (Assistant Professor, Vascular/UW Medicine-Montlake)
The council was also responsible for creating a policy that more clearly defined standards around pregnancy, paternal leave, and lactation issues for both faculty and residents. Issues for the pregnant surgeon such as when call, clinic, and elective surgery scheduling can stop were defined, as were clearer standards regarding leave time for all genders, as well as for those adding children to their families in ways other than directly giving birth to them. The information contained within the policy and the knowledge gained from discussions about it were helpful to Dr. Douglas Wood, The Henry N. Harkins Professor and Chair, during his work as a member of the American College of Surgeons' (ACS) committee that drafted a statement on pregnancy, parental leave and workplace accommodations for surgical trainees in 2020.
Currently, the council is working on the development of a sponsorship program, as well as addressing ongoing issues that impact the success of breast feeding among women surgeons. We also continue our academic pursuits, investigating whether gender-based differences in medical student or resident assessment exist. Our initial work was published a research letter in JAMA Surgery in 2022. We look forward to continuing to work to ensure gender equity in the department.
Initially, part of the overall Women’s Council, the Resident Women’s Council, was created in 2018 when it became apparent that specific issues impacting women at the faculty and training levels were different enough to justify a separate council. The current council includes women residents from General Surgery, Vascular Surgery, Cardiothoracic and Plastic Surgery from the intern through the chief resident level. The UW DOS Resident Women's Council empowers and supports residents with the goal of promoting gender equity in surgery.
Current resident council members:
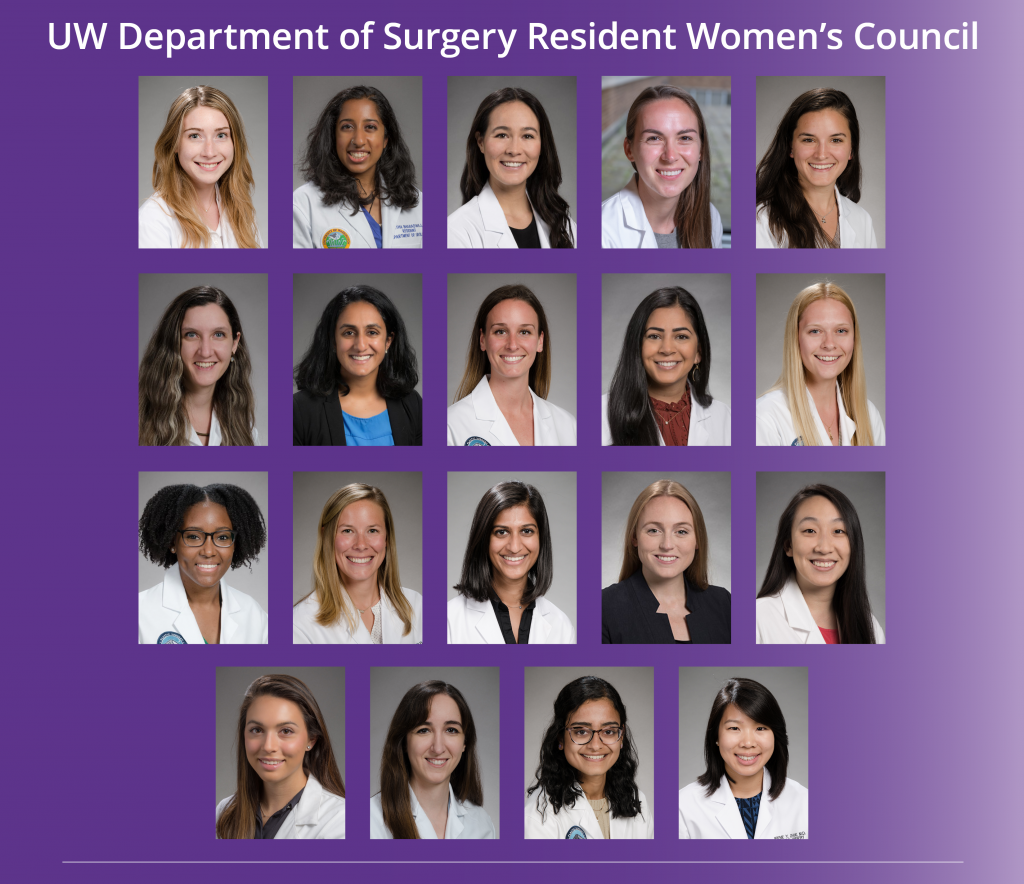
Top row: Cat Beni - General Surgery resident, Maheetha Bharadwaj - Urology resident, Malia Brennan - General Surgery resident, Katy Chan - General Surgery resident, Nina Clark - General Surgery resident
Second row: Giulia Daneshgaran - Plastic Surgery resident, Mohini Dasari - Transplant Surgery fellow, Rebecca DeSanti - Plastic Surgery resident, Karanpreet Dhaliwal - Cardiothoracic Surgery resident, Danielle Eble – Plastic Surgery resident (Chair)
Third row: Shanique Martin - Plastic Surgery resident, Kate McNevin - General Surgery resident, Kajal Mehta - General Surgery resident, Blake Murphy - Vascular Surgery resident, Abra Shen - Plastic Surgery resident
Fourth row: Mahsa Taskindoust - Plastic Surgery resident, Editt Taslakian - Plastic Surgery resident, Nikki Thrikutam - Plastic Surgery resident, Irene Zhang - General Surgery resident
Projects have focused on fostering mentorship opportunities between DOS faculty and residents, fostering mentorship between residents and UW SOM medical students interested in surgery, and conducting research projects related to advancing gender equity in surgery. The UW DOS Resident Women’s Council has devoted significant time to fostering relationships with UW SOM medical students interested in surgical careers. The council originated a mentorship program that matches medical students starting as early as the MS1 year with residents in their surgical field of interest. The pairs meet frequently and give perspective surgical applicants access to someone who can truly give them guidance and honest answers to career questions that arise. In addition to this formalized mentorship program, the resident council members have worked closely with the UW SOM Association of Women Surgeons (AWS) chapter. They co-hosted an informational panel session entitled “So you want to be a surgeon” in September 2022 and have conducted mock residency interviews for medical students applying in a surgical field. Social gatherings have happily returned as the pandemic continues to wane.

Informational Panel “Life as a Surgeon” for UW School of Medicine medical students.
Academically the council co-sponsored a project investigating the impact of gender on grading within our multi-site, multi-state surgical clerkship. This work was accepted as a poster for presentation at the Association of Surgical Education Annual meeting during Surgical Education Week which occurred virtually due to the Covid-19 Pandemic in April 2020 and was published in the Journal of Surgical Education in 2022.
The UW Women in Surgery group brings together faculty and trainee surgeons from across the DOS surgical specialties as a community. This group meets regularly throughout the year for various events, often hosted by a faculty or resident surgeon. We believe strongly in and cherish our community. By coming together, we connect and learn from each other, benefitting both our professional and personal lives.
Our activities thus far have included social events such as happy hours, holiday parties and Secret Santa exchanges, journal and article review-based discussions, discussions surrounding professional advancement, and wellness events such as joint Pilates classes.
The activities and events are currently coordinated by DOS General Surgery Resident Physicians Drs. Kajal Mehta and Dani Eble, with the input and support of numerous DOS faculty and residents.

Women in Surgery 2022 Social Gathering

Women in Surgery members in Women in Surgery caps

Women in Surgery members at 2022 holiday gathering
The UW DOS Faculty Women's Council’s main goal is to promote gender equity in surgery. One of the faculty council’s ongoing projects is the development of a sponsorship program for the department. The sponsorship program is being designed as another way to promote individuals at all levels and all genders at the local, regional and national level. Meant to work in parallel with the more formalized mentoring programs within various divisions, the goal of the sponsorship program will be to connect individuals with opportunities (see section below) of interest as they arise in a mutually beneficial relationship.
We also look forward to hosting the DOS Grand Rounds in March.
Current UW DOS Resident Council events include:
- Quarterly advice series on career development and job negotiation targeted at resident trainees with a variety of speakers.
- Mentorship program
- Surgical cap sale
- Monthly social events
While the Faculty and Resident Women’s Councils represent a fraction of the women in the department, we are highlighting our member’s recent accomplishments below.
APPOINTMENTS AND ELECTIONS
Dr. Erika Bisgaard joined the DOS as an Assistant Professor of Trauma, Burn, and Critical Care Surgery.
Dr. Erika Bisgaard was appointed Assistant program director of the SCC fellowship.
Dr. Eileen Bulger served as President of the American Association for the Surgery of Trauma.
Dr. Kristine Calhoun was appointed Director of the OSCE Program at UW SOM.
Dr. Judy Chen was appointed Affiliate Faculty for the UW Division of Health care Simulation Science.
Dr. Judy Chen served as Program Chair for the ACS WA and OR state chapter conference.
Dr. Shannon Colohan was appointed medical director of the Center for Reconstructive Surgery.
Dr. Kristen Dansey joined the DOS as an Assistant Professor in the Division of Vascular Surgery.
Dr. Sarah Greenberg was appointed Liaison for the American Academy of Pediatrics Section on Surgery to the Section on Global Health.
Dr. Sarah Greenberg was appointed General Surgery Lead for the SCH Surgical Services Research Council.
Dr. Sara Javid was promoted to Professor of Surgery July 2022.
Dr. Catherine Kling was elected the UNOS Region 6 Associate Councilor and Region 6 Representative to the UNOS Membership and Professional Standards Committee Representative.
Dr. Catherine Kling was appointed Vice Chair of the ASTS TACC Fellowship Program Accreditation Committee.
Dr. Deborah Marquardt was elected to attend the ACS Surgeon as Educators course.
Dr. Kajal Mehta, General Surgery resident was appointed Chair of RAS-ACS Global Surgery Working Group AY for the 2022-2023 academic year.
Dr. Kajal Mehta, General Surgery resident was named Co-chair, UW Department of Surgery Resident Women’s Council.
Dr. Emily Palmquist joined the Breast Surgery Service at UW SOM as an Assistant Professor of Surgery.
Dr. Zoe Parr was promoted to Clinical Associate Professor of Surgery in July 2022.
Dr. Rebecca Petersen served as 2023 SAGES Program Chair.
Dr. Rebecca Petersen was elected to SAGES Board of Governors.
Dr. Rebecca Petersen was appointed an Abdominal Core Health Quality Collaborative (ACHQC) Board Member.
Dr. Rebecca Petersen was appointed Interim Director, Residency Programs in General & Preliminary Surgery at UW SOM.
AWARDS
Dr. Eileen Bulger received the Norman McSwain Leadership Award from the National Association of Emergency Medical Technicians.
Dr. Eileen Bulger was recognized for her Outstanding Contributions to International Trauma Care, Academy of Sciences Saudi Arabia.
Dr. Mohini Dasari, General Surgery resident was awarded the David Tapper Award for Outstanding Junior Resident and Medical Student Education in June 2022.
Dr. Meghan Flanagan was selected to participate in the 2023 Medical Leadership Development High Potentials Program through the Fred Hutchinson Cancer Center.
Dr. Teresa Kim was selected to be in the inaugural cohort of the NIH/NCI Early-stage Surgeon Scientist Program (ESSP).
Dr. Teresa Kim was selected as the inaugural West Coast.
Dr. Blake Murphy, Vascular Surgery resident was the 37th Annual Western Vascular Society Meeting Rapid Fire Competition Winner for her oral presentation entitled “Aortic Size Index Accounts for Sex-Specific Differences In Abdominal Aortic Aneurysm Diameter At The Time of Rupture.”
Dr. Abra Shen, Plastics resident was named one of the Association of Women Surgeons Top 40 Under 40. (2022): https://www.womensurgeons.org/page/AWS40Under40
FAMILY
Dr. Emily Palmquist welcomed a daughter in December 2021.
Dr. Danielle Eble became engaged to Dr. Arjune Dhanekula in July 2022.
Dr. Sarah Goldsberry-Long welcomed her second child, a daughter.
Dr. Abra Shen, Plastic resident is expecting her first child January 2023.
FELLOWSHIPS
Dr. Erika Bisgaard completed her fellowship in Trauma/Critical Care.
Dr. Mohini Dasari started an Abdominal Transplant Surgery fellowship.
Dr. Deborah Marquardt completed a Surgical Education Fellowship through the Association of Surgical Education.
Dr. Emily Palmquist completed her fellowship in Breast Surgery.
GRANTS
Dr. Eileen Bulger was awarded funding for a project entitled “A Deployment Focused Pragmatic Trial of Optimal Stepped Care Intervention Targeting PTSD and Comorbidity for Acutely Hospitalized Injury Survivors in US Trauma Care SystemsCo.”
Dr. Sara Javid was awarded funding from the Department of Defense for a project entitled “Prevention of Lethal Metastatic Breast Cancer by Identifying and Eradicating Clinically Relevant Disseminated Tumor Cells.”
Dr. Teresa Kim was awarded the NIH/NCI Early-stage Surgeon Scientist Program (ESSP), 3-year grant for work entitled “Defining the Mechanism and Reversibility of IL-10-Driven Macrophage Polarization in Human Liver Metastasis.”
PRESENTATIONS AND PUBLICATIONS
Sobol D, Berfield K, Shalhub S, Tatum R, Yale L, Perkins J, Calhoun K. Exploring the Influence of Gender on Surgical Clerkship Grades and Test Scores: A Single Institution, Multisite Comparison. Journal of Surgical Education, Sep-Oct;79(5):1132-1139. doi: 10.1016/j.jsurg.2022.05.008. Epub 2022 Jun 1.PMID: 35660307
Bisgaard E. “Defining surgical culture.” American College of Surgeons presentation, San Diego
Meier JB, Stevens A, Isenberg E, Bisgaard EK, Abdelfattah KR, Balentine C. “Resident participation in general surgery procedures does not exacerbate disparities in outcomes”. Am J Surg. 10 Jan 23.
Gibran NS, Shipper E, Phuong J, Braverman M, Bixby P, Price MA, Bulger EM; NTRAP Burns & Reconstructive Surgery Panel Group. Developing a national trauma research action plan: Results from the Burn Research Gap Delphi Survey. J Trauma Acute Care Surg. 2022 Jan 1;92(1):201-212. doi: 10.1097/TA.0000000000003409. PMID: 34554139.
Fischer PE, Gestring ML, Sagraves SG, Michaels HN, Patel B, Dodd J, Campion EM, VanderKolk WE, Bulger EM. The national trauma triage protocol: how EMS perspective can inform the guideline revision. Trauma Surg Acute Care Open. 2022 Jan 18;7(1):e000879. doi: 10.1136/tsaco-2021-000879. PMID: 35128069; PMCID: PMC8768919.
Herrera-Escobar JP, Price MA, Reidy E, Bixby PJ, Hau K, Bulger EM, Haider AH; National Trauma Research Action Plan (NTRAP) Long-term Patient-Reported Outcomes Panel. Core Outcome Measures for Research in Traumatic Injury Survivors: The NTRAP Modified Delphi Consensus Study. J Trauma Acute Care Surg. 2022 Jan 25. doi: 10.1097/TA.0000000000003546. Epub ahead of print. PMID: 35081596.
McDade JE, Deming HC, Jinks-Chang S, Paulsen MR, Bui AL, Vavilala MS, Rivara FP, Bulger EM. Stop the Bleed Training for High School Students: Guardian Attitudes and Their Association with Prior Trauma. J Sch Health. 2022 Jan 30. doi: 10.1111/josh.13134. Epub ahead of print. PMID: 35098532.
Maughan BC, Lin A, Caughey AB, Bulger EM, McConnell KJ, Malveau S, Griffiths D, Newgard CD. Field Trauma Triage among Older Adults: A Cost-Effectiveness Analysis. J Am Coll Surg. 2022 Feb 1;234(2):139-154. doi: 10.1097/XCS.0000000000000025. PMID: 35213435.
Newgard CD, Braverman MA, Phuong J, Shipper ES, Price MA, Bixby PJ, Goralnick E, Daya MR, Lerner EB, Guyette FX, Rowell S, Doucet J, Jenkins P, Mann NC, Staudenmayer K, Blake DP, Bulger EM; NTRAP Prehospital and Mass Casualty Preparedness Panel Group. Developing a National Trauma Research Action Plan: Results from the prehospital and mass casualty research Delphi survey. J Trauma Acute Care Surg. 2022 Feb 1;92(2):398-406. doi: 10.1097/TA.0000000000003469. PMID: 34789701.
Stewart BT, Mehta K, Drago M, Henry S, Joseph K, Strong K, Trostchansky JL, Jorgensen JJ, Leung GK, Abi-Saad GS, Bulger E, Mock C. Global Survey of Demand-Side Factors and Incentives that Influence Advanced Trauma Life Support (ATLS) Promulgation. World J Surg. 2022 Feb 6. doi: 10.1007/s00268-022-06461-9. Epub ahead of print. PMID: 35128569.
Bulger EM, Johnson P, Parker L, Moloney KE, Roberts MK, Vaziri N, Seo S, Nehra D, Thomas P, Zatzick D. Nationwide Survey of Trauma Center Screening and Intervention Practices for Posttraumatic Stress Disorder, Firearm Violence, Mental Health, and Substance Use Disorders. J Am Coll Surg. 2022 Mar 1;234(3):274-287. doi: 10.1097/XCS.0000000000000064. PMID: 35213489.
Hamad DM, Mandell SP, Stewart RM, Patel B, Guttman MP, Williams P, Thomas A, Jerath A, Bulger EM, Nathens AB. Error reduction in trauma care: Lessons from an anonymized, national, multicenter mortality reporting system. J Trauma Acute Care Surg. 2022 Mar 1;92(3):473-480. doi: 10.1097/TA.0000000000003485. PMID: 34840270.
Lupton JR, Davis-O'Reilly C, Jungbauer RM, Newgard CD, Fallat ME, Brown JB, Mann NC, Jurkovich GJ, Bulger E, Gestring ML, Lerner EB, Chou R, Totten AM. Under-Triage and Over-Triage Using the Field Triage Guidelines for Injured Patients: A Systematic Review. Prehosp Emerg Care. 2022 Mar 4:1-8. doi: 10.1080/10903127.2022.2043963. Epub ahead of print. PMID: 35191799.
Conrick KM, Mills B, Mohamed K, Bulger EM, Arbabi S, Vil CS, Dotolo D, Solano E, Vavilala MS, Rowhani-Rahbar A, Moore M. Improving Data Collection and Abstraction to Assess Health Equity in Trauma Care. J Med Syst. 2022 Mar 9;46(4):21. doi: 10.1007/s10916-022-01804-4. PMID: 35260929.
Lupton JR, Davis-O'Reilly C, Jungbauer RM, Newgard CD, Fallat ME, Brown JB, Mann NC, Jurkovich GJ, Bulger E, Gestring ML, Lerner EB, Chou R, Totten AM. Mechanism of injury and special considerations as predictive of serious injury: A systematic review. Acad Emerg Med. 2022 Mar 23. doi: 10.1111/acem.14489. Epub ahead of print. PMID: 35319149.
Joseph B, Saljuqi AT, Phuong J, Shipper E, Braverman MA, Bixby PJ, Price MA, Barraco RD, Cooper Z, Jarman M, Lack W, Lueckel S, Pivalizza E, Bulger E; Geriatric Trauma Panel. Developing a National Trauma Research Action Plan: Results from the geriatric research gap Delphi survey. J Trauma Acute Care Surg. 2022 Aug 1;93(2):209-219. doi: 10.1097/TA.0000000000003626. Epub 2022 Apr 8. PMID: 35393380.
Senekjian L, Robinson BRH, Meagher AD, Gross JA, Maier RV, Bulger EM, Arbabi S, Cuschieri J. Nonoperative Management in Blunt Splenic Trauma: Can Shock Index Predict Failure? J Surg Res. 2022 Aug;276:340-346. doi: 10.1016/j.jss.2022.02.035. Epub 2022 Apr 12. PMID: 35427912.
Costantini TW, Galante JM, Braverman MA, Phuong J, Price MA, Cuschieri J, Godat LN, Holcomb JB, Coimbra R, Bulger EM; NTRAP Acute Resuscitation Panel. Developing a National Trauma Research Action Plan (NTRAP): Results from the Acute Resuscitation, Initial Patient Evaluation, Imaging, and Management Research Gap Delphi Survey. J Trauma Acute Care Surg. 2022 Apr 21. doi: 10.1097/TA.0000000000003648. Epub ahead of print. PMID: 35444148.
Newgard CD, Fischer PE, Gestring M, Michaels HN, Jurkovich GJ, Lerner EB, Fallat ME, Delbridge TR, Brown JB, Bulger EM; Writing Group for the 2021 National Expert Panel on Field Triage. National guideline for the field triage of injured patients: Recommendations of the National Expert Panel on Field Triage, 2021. J Trauma Acute Care Surg. 2022 Aug 1;93(2):e49-e60. doi: 10.1097/TA.0000000000003627. Epub 2022 Apr 27. PMID: 35475939; PMCID: PMC9323557.
Ali M, Liu Z, Taylor M, Orcutt T, Bledsoe A, Phuong J, Stansbury LG, Arbabi S, Robinson BRH, Bulger E, Vavilala MS, Hess JR. Blood product availability in the Washington state trauma system. Transfusion. 2022 Apr 26. doi: 10.1111/trf.16888. Epub ahead of print. PMID: 35470898.
Cooper Z, Herrera-Escobar JP, Phuong J, Braverman MA, Bonne S, Knudson MM, Rivara FP, Rowhani-Rahbar A, Price MA, Bulger EM; NTRAP Injury Prevention Panel. Developing a National Trauma Research Action Plan (NTRAP): Results from the Injury Prevention Research Gap Delphi Survey. J Trauma Acute Care Surg. 2022 May 12. doi: 10.1097/TA.0000000000003665. Epub ahead of print. PMID: 35545804.
Stein DM, Upperman JS, Livingston DH, Andrews J, Bulger EM, Cohen MJ, Eastridge BJ, Fontaine MJ, Guillamondegui O, Hess JR, Jenkins DH, Kaups KL, Nance ML, Spinella PC, Zarzaur BL, Zonies D, Coimbra R. National Blood Shortage: A Call to Action from the Trauma Community. J Trauma Acute Care Surg. 2022 May 25. doi: 10.1097/TA.0000000000003715. Epub ahead of print. PMID: 35610747.
Dumas RP, Bankhead BK, Coleman JR, Dhillon NK, Meizoso JP, Bessoff K, Butler WJ, Strickland M, Dultz LA, Davis K, Bulger EM, Reilly PM, Croce MA, Spain DA, Livingston DH, Brasel K, Coimbra R, Knowlton LM. Developing and Leading a Sustainable Organization for Early Career Acute Care Surgeons: Lessons from the Inaugural AAST Associate Member Council. J Trauma Acute Care Surg. 2022 Jul 1. doi: 10.1097/TA.0000000000003734. Epub ahead of print. PMID: 35777976.
Brasel KJ, Braverman MA, Phuong J, Price MA, Kaplan LJ, Kozar R, Michetti CP, Callcut R, Bulger EM, Callcut R, Codner P, Evans S, Kaplan LJ, Kim D, Kozar R, Lipsett P, Lissauer M, Maier RV, Martin ND, May AK, Michetti CP, Murray MJ, Napolitano L, Nirula R, Pittet JF, Robinson B, Rodgers RB, Thakkar R, Tisherman SA, West M, Zonies D; and the Postadmission Critical Care Research Panel Group. Developing a National Trauma Research Action Plan: Results from the postadmission critical care research gap Delphi survey. J Trauma Acute Care Surg. 2022 Dec 1;93(6):846-853. doi: 10.1097/TA.0000000000003754. Epub 2022 Aug 2. PMID: 35916626.
Herrera-Escobar JP, Reidy E, Phuong J, Brasel KJ, Cuschieri J, Fallat M, Potter BK, Price MA, Bulger EM, Haider AH; NTRAP Long-term Outcomes Panel. Developing a National Trauma Research Action Plan (NTRAP): Results from the Long-term Outcomes Research Gap Delphi Survey. J Trauma Acute Care Surg. 2022 Aug 16. doi: 10.1097/TA.0000000000003747. Epub ahead of print. PMID: 35972140.
Addams J, Arbabi S, Bulger EM, Stansbury LG, Tuott EE, Hess JR. How we built a hospital-based community whole blood program. Transfusion. 2022 Sep;62(9):1699-1705. doi: 10.1111/trf.17018. Epub 2022 Jul 11. PMID: 35815552.
Stein DM, Upperman JS, Livingston DH, Andrews J, Bulger EM, Cohen MJ, Eastridge BJ, Fontaine MJ, Guillamondegui O, Hess JR, Jenkins DH, Kaups KL, Nance ML, Spinella PC, Zarzaur BL, Zonies D, Coimbra R. National blood shortage: A call to action from the trauma community. J Trauma Acute Care Surg. 2022 Sep 1;93(3):e119-e122. doi: 10.1097/TA.0000000000003715. Epub 2022 May 25. PMID: 35610747.
Groner JI, Phuong J, Price MA, Bixby PJ, Ehrlich PF, Burd RS, Jensen AR, Rivara FP, Sribnick EA, Bulger EM. Developing a National Trauma Research Action Plan: Results from the Pediatric Research Gap Delphi Survey. J Trauma Acute Care Surg. 2022 Sep 1;93(3):360-366. doi: 10.1097/TA.0000000000003610. Epub 2022 Mar 14. PMID: 35293373.
Cooper Z, Herrera-Escobar JP, Phuong J, Braverman MA, Bonne S, Knudson MM, Rivara FP, Rowhani-Rahbar A, Price MA, Bulger EM; NTRAP Injury Prevention Panel. Developing a National Trauma Research Action Plan: Results from the injury prevention research gap Delphi survey. J Trauma Acute Care Surg. 2022 Sep 1;93(3):367-375. doi: 10.1097/TA.0000000000003665. Epub 2022 May 12. PMID: 35545804.
Dumas RP, Bankhead BK, Coleman JR, Dhillon NK, Meizoso JP, Bessoff K, Butler WJ, Strickland M, Dultz LA, Davis K, Bulger EM, Reilly PM, Croce MA, Spain DA, Livingston DH, Brasel KJ, Coimbra R, Knowlton LM. Developing and leading a sustainable organization for early career acute care surgeons: Lessons from the inaugural American Association for the Surgery of Trauma Associate Member Council. J Trauma Acute Care Surg. 2022 Oct 1;93(4):e143-e146. doi: 10.1097/TA.0000000000003734. Epub 2022 Jul 1. PMID: 35777976.
Thomas AC, Campbell BT, Subacius H, Orlas CP, Bulger E, Stewart RM, Stey AM, Jang A, Hamad D, Bilimoria KY, Nathens AB. National evaluation of the association between stay-at-home orders on mechanism of injury and trauma admission volume. Injury. 2022 Nov;53(11):3655-3662. doi: 10.1016/j.injury.2022.09.012. Epub 2022 Sep 13. PMID: 36167686; PMCID: PMC9467931.
Jacobs L, Keating JJ, Hunt RC, Butler FK, Pons PT, Gestring M, Bulger E, Eastman A, Kerby J, Hashmi Z, Fridling J, Inaba K, Matsushima K, Goralnick E, Melnitchouk N, Welten V. Stop the BleedⓇ. Curr Probl Surg. 2022 Oct;59(10):101193. doi: 10.1016/j.cpsurg.2022.101193. Epub 2022 Aug 6. PMID: 36253022.
Bulger EM. Women in Trauma Surgery: Advancing our Profession Through International Collaboration. Kirurgen 1-2022, page 38-39.
Kerby J, Bulger EM. The COT at 100: A Legacy of Improved Care for the Injured Patient. American College of Surgeons Bulletin. March 4, 2022 https://bulletin.facs.org/2022/03/the-cot-at-100-a-legacy-of-improved-care-for-the-injured-patient/
Zern N, Yale L, Whipple M, Allen S, Wood D, Tatum R, Perkins J, Calhoun K. The Impact of the COVID-19 Pandemic on Medical Student Education: Implementation and Outcome of a Virtual General Surgery Curriculum. Am J Surg. 2022 Jul;224(1 Pt B):612-616. doi: 10.1016/j.amjsurg.2022.03.035. Epub 2022 Mar 26.PMID: 35361472
Sobol D, Berfield K, Shalhub S, Tatum R, Yale L, Perkins J, Calhoun K. Exploring the Influence of Gender on Surgical Clerkship Grades and Test Scores: A Single Institution, Multisite Comparison. Journal of Surgical Education, Sep-Oct;79(5):1132-1139. doi: 10.1016/j.jsurg.2022.05.008. Epub 2022 Jun 1.PMID: 35660307
Crary IL, Parker EU, Lowry KP, Patwardhan PP, Soong TR, Javid SH, Calhoun KE, Flanagan MR.. Risk of lobular neoplasia upgrade with synchronous carcinoma. Ann Surg Oncol. 2022 Oct;29(10):6350-6358. doi: 10.1245/s10434-022-12129-4. Epub 2022 Jul 8.PMID: 35802213
Purdy AC, Smith BR, Amersi F, Calhoun KE, Lewis RJ, Tolles J, Dauphine C, Roy M, Jarman BT, Han A, Neville AL, Dickinson KJ, Salcedo E, Frey ES, Poola VP, Murayama KM, Chen F, Yung E, de Virgilio C; Surgery Educators Group. Characteristics Associated with Outstanding General Surgery Residency Graduate Performance, as Rated by Surgical Educators. JAMA Surg. 2022 Aug 10:e223340. doi: 10.1001/jamasurg.2022.3340. Online ahead of print.PMID: 35947371
Anderson JE, Zern NE, Calhoun KE, Wood DE, Smith CA. Assessment of Potential Gender Bias in General Surgery Resident Milestone Evaluations. JAMA Surg. 2022 Oct 12:e223929. doi: 10.1001/jamasurg.2022.3929. Online ahead of print.PMID: 36223104.
Annual Research Symposium and Helen and John Schilling Lecture, University of Washington, Seattle, WA. Oral Presentation. March 25, 2022. Perceptions of Surgical Careers from the Female Medical Student Perspective. DeSanti R, Liu Y, Herrin M, Colohan S, Calhoun K. (Abstract).
Clark NM, Roberts EA, Federenko C, Sun Q, Dubard-Gault M, Handford C, Yung R, Cheng HH, Sham JG, Norquist BM, Flanagan MR. ASO Visual Abstract: Genetic testing among patients with high-risk breast, ovarian, pancreatic and prostate cancers. Ann Surg Oncol, Published online November 22, 2022.
Ha M, Ngaage LG, Finkelstein ER, Klein M, Yanga A, Colohan SM, Nurudeen SM, Terhune JH, Slezak S, Rasko YM. Insurance Coverage of Prophylactic Mastectomies: A National Review of the United States. Clin Breast Cancer. 2022 Dec 5:S1526-8209(22)00269-5.
Annual Research Symposium and Helen and John Schilling Lecture, University of Washington, Seattle, WA. Oral Presentation. March 25, 2022. Perceptions of Surgical Careers from the Female Medical Student Perspective. DeSanti R, Liu Y, Herrin M, Colohan S, Calhoun K. (Abstract).
Weinberg M, Heiman A, DeSanti R, Lanni MA, Vankouwenberg E, Patel A. Outcomes of the Keystone Island Perforator Flap: A Systematic Review. Journal of Reconstructive Microsurgery. 2022 November; 38(9): 727-733. PMID: 35477115. https://doi.org/10.1055/s-0042-1745744
Plastic Surgery Research Council, Toronto, Canada. Poster Presentation. June 8-12, 2022. Characterization of Upper Extremity Firearm Injuries in the Adult Population. DeSanti RL, Yu JL, Keys KA, Friedrich JB. (Abstract).
Annual Research Symposium and Helen and John Schilling Lecture, University of Washington, Seattle, WA. Oral Presentation. March 25, 2022. Perceptions of Surgical Careers from the Female Medical Student Perspective. DeSanti R, Liu Y, Herrin M, Colohan S, Calhoun K. (Abstract).
Cockrell HC, Greenberg SLM, Knight JA, Green NF, Romberg ER, Bonilla-Velez J. Magnetic Resonance Imaging of Children Following Esophageal Button Battery Removal: What are we looking for? Clinical Imaging. 2022 June;86:71-74.
Anderson JE, Taylor MR, Romberg EK, Riehle KJ, Kapur R, Crocker ME, Crotty EE, Hergenroeder G, Greenberg SLM. Mature mediastinal teratoma with tumor rupture into airway. Journal of Pediatric Surgery Case Reports. 2022 June;81:102270.
Truche P, Smith ER, Ademuyiwa A, Buda A, Nabukenya MT, Kaseje N, Ameh EA, Greenberg S, Evans F, Bickler S, Meara JG, Rice HE. Defining Surgical Workforce Density Targets to Meet Child and Neonatal Mortality Rate Targets in the Age of the Sustainable Development Goals: A Global Cross-Sectional Study. World J Surg. 2022 Sep;46(9):2262-2269.
Cockrell HC, Maine RG, Hansen EE, Mehta K, Salazar DR, Steward BT, Greenberg SLM. Environmental Impact of Telemedicine Use for Pediatric Surgery. J Pediatr Surg. 2022 Jul 7:S0022-3468(22)00443-2.
Kamath A, Gentry K, Dawson-Hahn E, Ross F, Chiem J, Patrao F, Greenberg S, Ibrahim A, Jimenez N. Tailoring the Perioperative Surgical Home for Children in Refugee Families. International Anesthesiology Clinics. 2022 Nov. Online ahead of print. doi: 10.1097/AIA.0000000000000387
Greenberg SLM, Cockrell HC, Hyman G, Goodman L, Kaseje N, Oldham K. The Global Initiative for Children’s Surgery: conception, gestation and delivery. Pediatr Surg Int. 2023 Dec;39(48). Online ahead of print. doi: 10.1007/s00383-022-05319-4
Lin B, Eble DJ, Riley MS, He K, Kristo G. Omental flap as a novel alternative technique for closure of a left para-duodenal hernia defect: A case report. ACS Case Reviews in Surgery. Accepted for publication on May 13, 2021.
Liu Y, Miller EA, Wee CE, Prsic A, Eble DJ, Kao DS. Osteoplastic Thumb Reconstruction in the Immediate Setting: A Case Series. Plas Reconstr Surg Glob Open. 2022 Jun 14;10(6):e4385. PMID 35720199.
Tolley PD, Yu J, Cho D, Thrikutam N, Eble DJ, Shih J, Leonhard V, Friedrich JB. Evaluating the ACAPS Standardized Letter of Recommendation for Application to Plastic Surgery Residency: Usefulness and Patterns. Plast Reconstr Surg. Accepted for publication on Dec 3, 2021.
Flanagan MR. Six early symptoms of breast cancer that are too easy to miss. Self Magazine, October 24, 2022. https://www.self.com/story/early-symptoms-of-breast-cancer
Jordahl KM, Malone KE, Baglia ML, Flanagan MR, Tang M-TC, Porter PL, Li CI. Alcohol consumption, smoking and invasive breast cancer risk after ductal carcinoma in situ. Breast Cancer Research and Treatment. Published online March 27, 2022.
Lam DL, Flanagan MR. Axillary adenopathy after COVID-19 vaccination in a Woman with Breast Cancer. JAMA. 2022; 327(2):175-176.
Miller T, Flanagan MR, Lowry K, Kilgore M. Error reduction and diagnostic concordance in breast pathology. Surgical Pathology Clinics. 2022; 15(1):1-13.
Flanagan MR, Doody DR, Voutsinas J, Wu Q, Banda K, Sharifi N, Li CI, Gadi VK. Association of HSD3B1 genotype and clinical outcomes in postmenopausal estrogen-receptor positive breast cancer. Ann Surg Oncol. Published online July 1, 2022.
Crary IL, Parker EU, Lowry KP, Patwardhan PP, Soong TR, Javid SH, Calhoun KE, Flanagan MR. Risk of lobular neoplasia upgrade with synchronous carcinoma. Ann Surg Oncol. Published online July 8, 2022.
Kim JN, Yung R, Lin Y, Meyer J, Kwon Y, Flanagan MR. Breast Cancer Therapy and Huntington Disease: A case report. Advances in Radiation Oncology. Published online July 15, 2022.
Crary IL, Parker EU, Lowry KP, Patwardhan PP, Soong TR, Javid SH, Calhoun KE, Flanagan MR. ASO Visual Abstract: Risk of lobular neoplasia upgrade with synchronous carcinoma. Ann Surg Oncol. Published online July 20, 2022.
Flanagan MR, Doody DR, Voutsinas J, Wu Q, Banda K, Sharifi N, Li CI, Gadi VK. ASO Visual Abstract: Association of HSD3B1 genotype and clinical outcomes in postmenopausal estrogen-receptor positive breast cancer. Ann Surg Oncol. Published online August 18, 2022.
Clark NM, Roberts EA, Federenko C, Sun Q, Dubard-Gault M, Handford C, Yung R, Cheng HH, Sham JG, Norquist BM, Flanagan MR. Genetic testing among patients with high-risk breast, ovarian, pancreatic and prostate cancers. Ann Surg Oncol, Published online November 5, 2022.
Clark NM, Roberts EA, Federenko C, Sun Q, Dubard-Gault M, Handford C, Yung R, Cheng HH, Sham JG, Norquist BM, Flanagan MR. ASO Visual Abstract: Genetic testing among patients with high-risk breast, ovarian, pancreatic and prostate cancers. Ann Surg Oncol, Published online November 22, 2022.
Javid S. Fred Hutch Cancer Center Blog. A trio of new approaches for breast cancer surgery. September 23, 2022. https://www.seattlecca.org/story/a-trio-of-new-approaches-for-breast-cancer-surgery
Javid S. Cancer Pathways Encompassing Cancer Podcast: Feel for lumps, save your bumps: breast self awareness with Dr. Sara Javid. October 2022. https://podcasts.apple.com/us/podcast/feel-for-lumps-save-your-bumps-breast-self-awareness/id1616721257?i=1000582149186
Javid S. Fred Hutchinson Cancer Center, Seattle WA. “Science Says: Three for 2023: Collaborations that Inspire Us”. Blue Jeans Virtual Event. November 29, 2022.
Crary IL, Parker EU, Lowry KP, Patwardhan PP, Soong RT, Javid SH, Calhoun KE, Flanagan MR. Risk of lobular neoplasia upgrade with synchronous carcinoma. Ann Surg Oncol. 2022; Epub 2022 Jul 8.PMID: 35802213
Gradishar WJ, Moran MS, Abraham J, Aft R, Agnese D, Allison KH, Anderson B, Burstein HJ, Chew H, Dang C, Elias AD, Giordano SH, Goetz MP, Goldstein LJ, Hurvitz SA, Isakoff SJ, Jankowitz RC, Javid SH, Krishnamurthy J, Leitch M, Lyons J, Mortimer J, Patel SA, Pierce LJ, Rosenberger LH, Rugo HS, Sitapati A, Smith KL, Smith ML, Soliman H, Stringer-Reasor EM, Telli ML, Ward JH, Wisinski KB, Young JS, Burns J, Kumar R. Breast Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022 Jun;20(6):691-722. PMID: 35714673
Christensen DM, Shehata MN, Javid SH, Rahbar H, and Lam DL. Preoperative Breast MRI: Current Evidence and Patient Selection. Submitted Journal of Breast Imaging. Accepted publication October 2022
Crary IL, Parker EU, Lowry KP, Patwardhan PP, Soong TR, Javid SH, Calhoun KE, Flanagan MR. ASO Visual Abstract: Risk of lobular neoplasia upgrade with synchronous carcinoma. Ann Surg Oncol. Oct;29(10):6360. PMID: 35857198
ASBrS Committee on Axillary Management: Cody HS, Snider H, Schwartz T, Rosenkranz KM, James TA, Alvarado M, Boughey JC, Javid S, Giuliano AE, Margenthaler JA, Moran MS, Rao R, Wilke LG. ASBrS Official Statement: Consensus guideline on axillary management for patients with in situ and invasive breast cancer: a concise overview. Published online March 14, 2022.
Goff PH^, Riolobos L^, LaFleur BJ, Spraker MB, Seo YD, Smythe KS, Campbell JS, Pierce RH, Zhang Y, He Q, Kim EY, Schaub SK, Kane GM, Mantilla JG, Chen EY, Ricciotti R, Thompson MJ, Cranmer LD, Wagner MJ, Loggers ET, Jones RL, Murphy E, Blumenschein WM, McClanahan TK, Earls J, Flanagan KC, LaFranzo NA, Kim TS^, Pollack SM^. Neoadjuvant therapy induces a potent immune response to sarcoma, dominated by myeloid and B cells. Clinical Cancer Research. 2022 Feb 3, epub ahead of print. Cited in PubMed; PMID 35115306. ^These authors contributed equally. [original work]
Veatch JR, Lee SM, Shasha C, Singhi N, Szeto JL, Moshiri AS, Kim TS, Smythe K, Kong P, Fitzgibbon M, Jesernig B, Bhatia S, Tykodi S, Hall ET, Byrd DR, Thompson JA, Pillarisetty VG, Duhen T, Houghton AM, Newell E, Gottardo R, Riddell SR. Neoantigen-specific CD4+ T cells in human melanoma have diverse differentiation states and correlate with CD8+ T cell, macrophage, and B cell function. Cancer Cell. 2022 Apr 11; 40(4): 393-409.e9. Cited in PubMed; PMID 35413271. [original work]
Sullivan KM^, Jiang X^, Guha P, Lausted C, Carter JA, Hsu C, Labadie KP, Kohli K, Kenerson HL, Daniel SK, Yan X, Meng C, Abbasi A, Chan M, Seo YD, Park JO, Crispe IN, Yeung RS, Kim TS, Gujral TS, Tian Q, Katz SC, Pillarisetty VG. Blockade of interleukin 10 potentiates antitumor immune function in human colorectal cancer liver metastases. Gut. 2022 June 15, epub ahead of print. Cited in PubMed; PMID 35705369. ^These authors contributed equally. [original work]
Sharma AK, Kim TS, Bauer S, Sicklick JK. Gastrointestinal Stromal Tumor: New Insights for a Multimodal Approach. Surgical Oncology Clinics of North America. 2022 Jul;31(3):431-446. Cited in PubMed; PMID 35715143. [review]
Voillet V, Berger TR, McKenna KM, Paulson KG, Tan WH, Smythe K, Hunter DS, Valente WJ, Weaver S, Campbell JS, Kim TS, Byrd DR, Bielas JH, Pierce RH, Chapuis AG, Gottardo R, Rongvaux A. An in vivo model of human macrophages in metastatic melanoma. Journal of Immunology. 2022 Jul 11;ji2101109, epub ahead of print. Cited in PubMed; PMID 35817516. [original work]
Noh S, Nessim C, Keung EZ, Roland CL, Strauss D, Sivarajah G, Fiore M, Biasoni D, Cioffi SPB, Mehtsun W, Canazi FCM, Sicoli F, Quagliuolo V, Chen J, Luo C, Gladd RA, Swallow C, Johnston W, Ford SJ, Evenden C, Tirotta F, Almond M, Nguyen L, Rutkowski P, Krotewicz M, Pennacchioli E, Cardona K, Gamboa A, Hompes D, Renard M, Kollar A, Ryser CO, Vassos N, Raut CP, Fairweather M, Krakorova DA, Quildrian S, Perhavec A, Nizri E, Farma JM, Greco S, Vincenzi B, Lopez JAG, Solerdecoll MS, Iwata S, Fukushima S, Kim T, Tolomeo F, Snow H, Howlett-Jansen Y, Tzanis D, Nikulin M, Gronchi A, Sicklick J, Transatlantic Australasian Retroperitoneal Sarcoma Working Group. Retrospective Analysis of Retroperitoneal-Abdominal-Pelvic Ganglioneuromas: An International Study by the Transatlantic Australasian Retroperitoneal Sarcoma Working Group. Annals of Surgery. 2022 Jul 22, online ahead of print. Cited in PubMed; PMID 35866666. [original work]
Marquardt D, Langdale L, Kim S, et al. Closing the gap: Triangulation of surgeons' respectful behaviors perceived by medical students, residents, and patients. Surgery. 2022;172(1):96-101. doi:10.1016/j.surg.2021.11.036
Wang TN, Shriki JE, Marquardt DL. Repeat Laparoscopic Cholecystectomy for Duplicated Gallbladder After 16-Year Interval. Fed Pract. 2022;39(2):e1-e5. doi:10.12788/fp.0213
Marquardt D, Langdale L, Kim S, et al. Closing the gap: Triangulation of surgeons' respectful behaviors perceived by medical students, residents, and patients. Surgery. 2022;172(1):96-101. doi:10.1016/j.surg.2021.11.036
Mesic A, Gyedu A, Mehta K, Goodman S, Mock C, Quansah R, Donkor P, Stewart B. Factors contributing to and reducing delays in the provision of adequate care in Ghana: a qualitative study of trauma care providers. Accepted in World Journal of Surgery, July 2022.
Cockrell H, Maine RG, Hansen EE, Mehta K, Rebollo-Salazar D, Stewart BT, Greenberg SLM. Environmental impact of telehealth use for pediatric surgery. Accepted in Journal of Pediatric Surgery, June 2022.
Gyedu A, Mehta K, Baidoo H, Addo H, Abdullah M, Mesic A, Sanosorn A, Cancio L, Yadav M, Nakarmi K, Stewart BT. Preferences for oral rehydration drinks among healthy individuals in Ghana: a single-blind, cross-sectional survey to inform implementation of an enterally based resuscitation protocol for burn injury. Burns. May 2022; DOI: 10.1016/j.burns.2022.05.016
Hebron C, Mehta K, Price T, Stewart BT, Potokar T. Lessons learned from the implementation of the WHO Global Burn Registry: barriers and facilitators to adoption, use and promulgation. Annals of Global Health. April 2022; DOI: 10.5334/aogh.3669
Stewart BT, Mehta K, Drago M, Henry S, Joseph K, Strong K, Trostchansky J, Jogensen J, Leung G, Abi-Saad G, Bulger E, Mock . Global Survey of Demand-Side Factors and Incentives that Influence Advanced Trauma Life Support (ATLS) Promulgation. World Journal of Surgery. 2022 Feb; DOI: 10.1007/s00268-022-06461-9
Mehta K, Arega H, Smith NL, Li K, Gause E, Meddings D, Stewart BT. Sex Differences in burn injuries, care and outcomes: a World Health Organization (WHO) Global Burn Registry cohort study. American Journal of Surgery. 2022 January; DOI: 10.1016/j.amjsurg.2021.07.041
Murphy B, Zettervall SL. Invited Commentary - Long-term Outcomes after FEVAR for Juxtarenal Aneurysms. [Sveinsson M, Sonesson B, Kristmundsson T, Dias N, Resch T. Long-term Outcomes after FEVAR for Juxtarenal Aortic Aneurysm.] In Press
Palmquist E, et al. Patient-Reported Outcome Measures for Patients Who Have Clinical T4 Breast Cancer Treated via Mastectomy with and Without Reconstruction. Ann Surg Oncol. 2022 Sep 23.
Shen AH, Shiah E, Sarac BA, Maselli AM, Nassar AH, Lee BT, Janis JE, Lin SJ. Plastic Surgery Residency Applicants' Perceptions of a Virtual Interview Cycle. Plastic and Reconstructive Surgery. 2022 Oct 1;150(4):930-939. Epub 2022 Aug 8. PMID: 35939639.
Shen AH, Alfonso AR, Cuccolo NG, Johnson AR, Lee BT, Lin SJ. Designing a Plastic and Reconstructive Surgery Virtual Curriculum (PRSVC): Assessment of Medical Student Knowledge, Surgical Skill, and Community Building. Plastic and Reconstructive Surgery. 2022 Sep 1;150(3):691-700. Epub 2022 Jul 13. PMID: 35819982.
Borrelli MR*, Griffin M*, Chen K, Deleon NMD, Adem S, Mascharak S, Shen AH, Ngaage LM, Lewis N, Longaker MT, Gurtner GC, Wan DC, Lorenz HP. Profibrotic Signaling Pathways and Surface Markers Are Upregulated in Fibroblasts of Human Striae Distensae and in a Mouse Model System. Plastic and Reconstructive Surgery. 2022 Aug 1;150(2):327-338. Epub 2022 Jun 6. PMID: 35666152.
Lane JC, Shen AH, Williams R, Gefter L, Friedman L, Zogg CK, Shaughnessy E; 2020-2021 Association of Women Surgeons National Medical Student Committee. If You Can See It, You Can Be It: Perceptions of Diversity in Surgery Among Under-Represented Minority High School Students. J Surg Educ. 2022 Apr 1:S1931-7204(22)00060-5. PMID: 35379582.
Hendele JB, Limaye AP, Sibulesky L. Misplaced emphasis, misunderstood risk: a cultural history of Public Health Service infectious disease guidelines. Curr Opin Organ Transplant. 2022 Apr 1;27(2):159-164. doi: 10.1097/MOT.0000000000000954. PMID: 35232929 Review.
Hendele JB, Perkins JD, Leca N, Biggins SW, Sibulesky L. Optimizing Risk Assessment In Simultaneous Liver and Kidney Transplant: Donor and Recipient Factors Associated With Improved Outcome. Transplant Proc. 2022 Apr;54(3):715-718. doi: 10.1016/j.transproceed.2021.11.035. Epub 2022 Mar 5. PMID: 35260244
Butiu M, Obrisca B, Sibulesky L, Bakthavatsalam R, Smith KD, Gimferrer I, Warner P, Ismail G, Leca N. Donor-derived Cell-free DNA Complements De Novo Class II DSA in Detecting Late Alloimmune Injury Post Kidney Transplantation. Transplant Direct. 2022 Jan 26;8(2):e1285. doi: 10.1097/TXD.0000000000001285. eCollection 2022 Feb. PMID: 35187211 Free PMC article.
Sibulesky L, Leca N, Limaye AP, Ramasamy B, Perkins JD. Survival Benefit in Older Patients Transplanted With Viremic Hepatitis C Positive Kidneys When Compared With High KDPI Kidneys. Transplantation. 2022 Nov 1;106(11):2217-2223. doi: 10.1097/TP.0000000000004179. Epub 2022 May 27. PMID: 35675439
Robinson TJ, Hendele JB, Gimferrer I, Leca N, Biggins SW, Reyes JD, Sibulesky L. Acute liver failure secondary to acute antibody mediated rejection after compatible liver transplant: A case report. World J Hepatol. 2022 Jan 27;14(1):287-294. doi: 10.4254/wjh.v14.i1.287. PMID: 35126855 Free PMC article.
Obrișcă B, Butiu M, Sibulesky L, Bakthavatsalam R, Smith KD, Gimferrer I, Warner P, Ismail G, Leca N. Combining donor-derived cell-free DNA and donor specific antibody testing as non-invasive biomarkers for rejection in kidney transplantation. Sci Rep. 2022 Sep 5;12(1):15061. doi: 10.1038/s41598-022-19017-7. PMID: 36064740 Free PMC article.
Anderson JE, Zern NE, Calhoun KE, Wood DE, Smith CA. Assessment of Potential Gender Bias in General Surgery Resident Milestone Evaluations. JAMA Surg. 2022 Oct 12:e223929. doi: 10.1001/jamasurg.2022.3929. Online ahead of print.PMID: 36223104.
Taskindoust M, Bowman T, Thomas SM, Levites H, Wickenheisser V, Hollenbeck ST. (2022). The Patient Narrative for Breast Implant Illness: A 10-Year Review of the U.S. Food and Drug Administration's MAUDE Database. Plastic and reconstructive surgery, 150(6), 1181–1187. https://doi.org/10.1097/PRS.0000000000009694
Rooney MM, Thomas SM, Taskindoust M, Greenup RA, Rosenberger LH, Hwang ES, Plichta JK. (2023). The role of tumor phenotype in the surgical treatment of early-stage breast cancer. American journal of surgery, 225(1), 84–92. https://doi.org/10.1016/j.amjsurg.2022.09.029
Shammas RL, Sergesketter AR, Taskindoust M, Biswas S, Hollenbeck ST, Phillips BT. (2022). Assessing the Influence of Failed Implant Reconstruction on Patient Satisfaction and Decision Regret after Salvage Free-Flap Breast Reconstruction. Journal of reconstructive microsurgery, 38(6), 441–450. https://doi.org/10.1055/s-0041-1735224
Hollins AW, Hein R, Atia A, Taskindoust M, Darner G, Shammas R, Mithani SK. (2022). Symptom Duration and Diabetic Control Influence Success of Steroid Injection in Trigger Finger. Plastic and reconstructive surgery, 150(2), 357e–363e. https://doi.org/10.1097/PRS.0000000000009320
Tolley PD, Yu J, Cho D, Thrikutam N, Eble DJ, Shih J, Leonhard V, Friedrich JB. Evaluating the ACAPS Standardized Letter of Recommendation for Application to Plastic Surgery Residency: Usefulness and Patterns. Plast Reconstr Surg. Accepted for publication on Dec 3, 2021.
Murphy B, Zettervall SL. Invited Commentary - Long-term Outcomes after FEVAR for Juxtarenal Aneurysms. [Sveinsson M, Sonesson B, Kristmundsson T, Dias N, Resch T. Long-term Outcomes after FEVAR for Juxtarenal Aortic Aneurysm.] In Press
