Abdominal Transplant Surgery
Abdominal Transplant Surgery
About the Program
The University of Washington Abdominal Transplant Surgery Fellowship is a two-year fellowship accredited by the American Society of Transplant Surgeons (ASTS). The program has been carefully designed to provide fellows with focused, hands-on training in Abdominal Transplant Surgery. Our program is defined by a culture of diversity and inclusion; we actively address healthcare inequities to support our mission of improving the health of the public and promote equity, diversity and inclusion across all aspects of transplant surgery care.
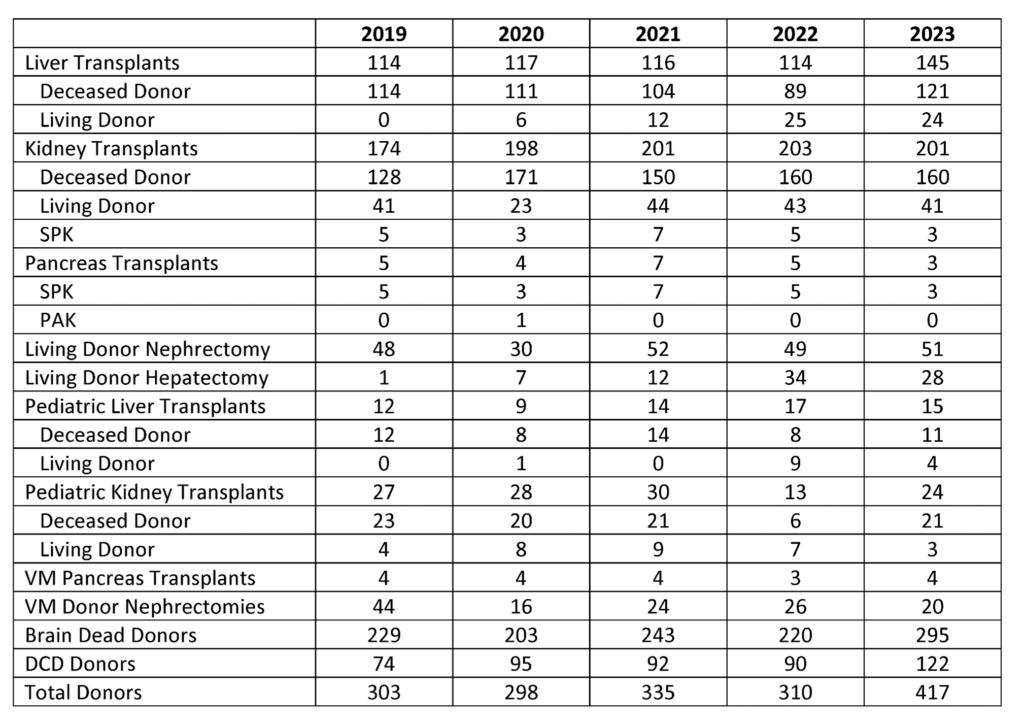
Throughout their training, fellows gain experience in:
- Operative techniques of deceased donor liver, kidney, and pancreas transplantation
- Operative techniques of living donor liver and kidney transplantation
- Deceased donor organ procurement (with a 20-30% rate of donation after circulatory death)
- Living donor hepatectomy and nephrectomy
- Fellows participate in the evaluation of donor offers
- Management and evaluation of transplant patients in the in and outpatient setting, including recipient and donor evaluations, post-operative management and management of immunosuppression and its complications
At the completion of this two-year program, fellows will be eligible for certification in liver and kidney transplantation. We are currently approved to match 3 fellows every two years. For the 2024 application cycle (with a fellowship start date of August 1, 2025) we have two open positions.
Program Leadership

Catherine Kling, MD MPH
Program Director,
Abdominal Transplant Fellowship
Assistant Professor, Transplant Surgery