Cardiothoracic Surgery-Integrated & 4/3 Programs
Cardiothoracic Surgery-Integrated & 4/3 Programs
About the Program
Established in 2010, the Cardiothoracic Surgery Integrated Residency program is dedicated to producing balanced, well-qualified cardiothoracic surgeons prepared to serve the community through careers in either private practice or academia. With dedicated faculty based at Seattle’s premier medical facilities, the program has been carefully designed to balance training in cardiovascular and thoracic surgery.
The residency is designed to provide residents with focused, hands-on experience divided equally between cardiac and thoracic surgery. While residents are welcome to choose an area of specialty, there are no pre-designated cardiac or thoracic tracks.
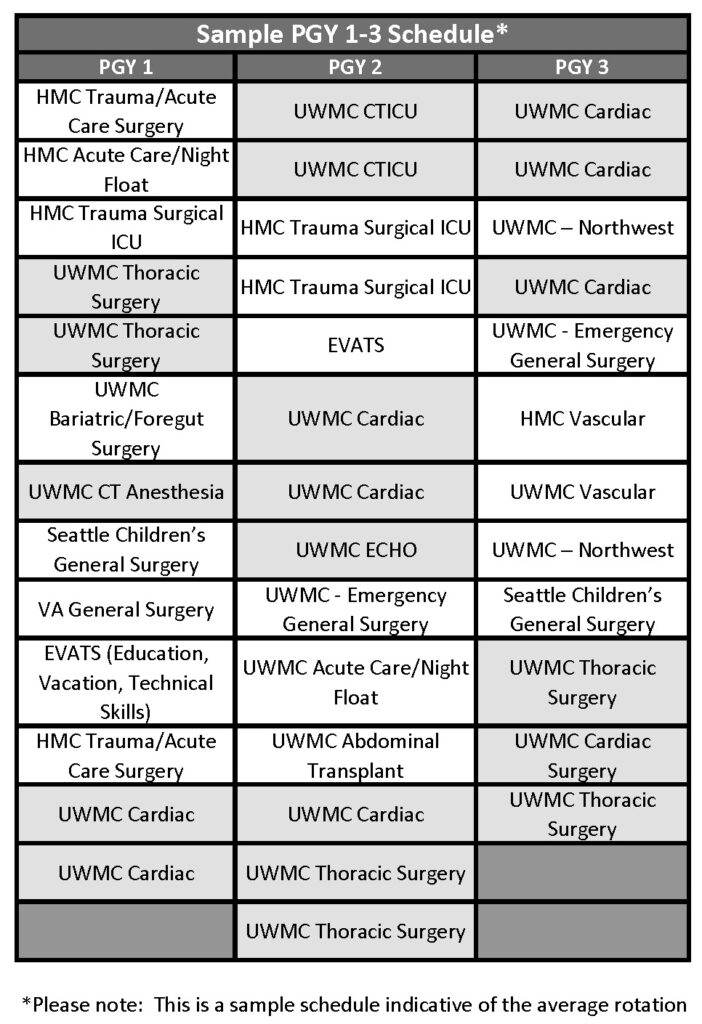
Integrated residents will spend their first three years of training (PGY 1-3) completing prerequisite clinical rotations including exposure to general surgery, vascular surgery, critical care, cardiothoracic surgery, echocardiography, and cardiothoracic anesthesia. Following this, senior Integrated residents (PGY 4-6) rotate on cardiothoracic surgery clinical services with fellows in the Cardiothoracic Surgery Fellowship program. In these latter years of training, residents will gain requisite experience in general thoracic, cardiac, congenital cardiac, and foregut surgery as well as end-stage heart and lung disease, including mechanical circulatory support and heart and lung transplantation.
Quick Facts
- Faculty have served as leaders of STS, ABS, ABTS, WTSA, TSDA, ACS, JCTSE, ISHLT, ELSO, and the ACGME Thoracic Surgery Residency Review Committee
- Division has completed 1000+ lung transplants and 900+ heart transplants.
- Average case numbers at graduation: 1575 total cases
Program Leadership
 Kathleen S. Berfield, MD |
 Christopher Ryan Burke, MD |
Clinical Experience
Integrated Cardiothoracic Surgery residents at the University of Washington receive an unrivaled clinical education. Training alongside nationally and internationally recognized faculty, residents have a robust operative experience in every subspecialty of cardiothoracic surgery from “bread and butter” cases” like CABGs and lobectomies to more complex cases like hybrid aortic aneurysm repair and pulmonary thromboendarterectomy.
What makes the Integrated program at the University of Washington unique is that it is one of the few programs in the country that trains you to be a true Cardiothoracic surgeon. Graduates are equipped to handle the full spectrum of cardiac and thoracic surgical disease. Additionally, as the tertiary and quaternary referral center for the WWAMI region, we care for a diverse patient population, which equates to a more robust clinical experience.
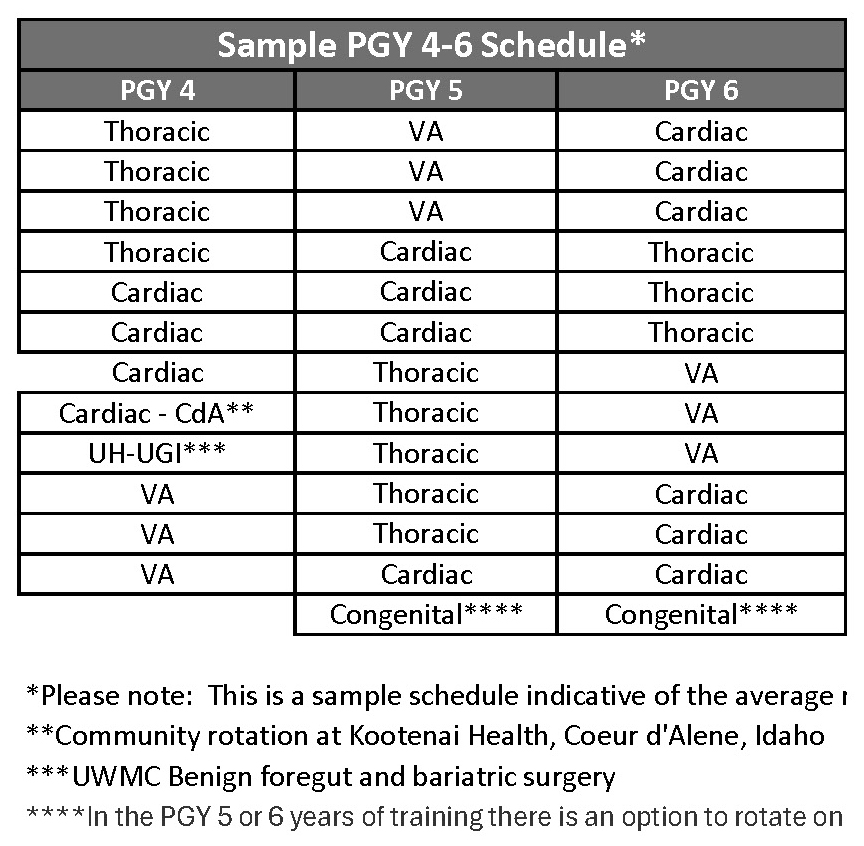
Residents spend their PGY 1-3 years building a foundation of surgical skills on a variety of specifically curated general surgery, vascular surgery, and cardiothoracic surgery rotations including cardiothoracic anesthesiology and echocardiography. The PGY 4-6 years are considered the “senior” years and are dedicated to perfecting technical skills and perioperative management of cardiothoracic surgical patients. Senior residents will primarily rotate on three services – UW Medical Center Thoracic Surgery, UW Medical Center Cardiac Surgery, Kootenai Health, and VA Cardiothoracic Surgery – gaining critical operative experience while working alongside leaders in the field.
Trainees in this program will have graduated autonomy from day one. Working in consultation with our Cardiothoracic Surgery faculty as well as partnering with advanced practice providers and perfusionists, residents in the Integrated Program are integral members of the team and oversee all aspects of perioperative care from the initial clinic visit until discharge, giving them a well-rounded education in clinical training.
Developing technical proficiency is at the core the Integrated Program’s mission. At the University of Washington, Cardiothoracic residents DO the cases, standing on the “surgeon’s side” of the table from day one. Throughout their six years of training residents participate in a myriad of simulation and surgical skills sessions aimed to help trainees hone their skills in everything from robotics to managing adverse intraoperative events.
Training Sites
Integrated Cardiothoracic Residents will rotate at six sites throughout their training.
- The University of Washington Medical Center–Montlake is a tertiary and quaternary care referral site for the WWAMI region and serves as the primary training site for the Integrated Program. Trainees in their PGY 1-3 years will spend about half their time at the UW Medical Center and it is the primary site of practice in the senior years of training.
- The VA Puget Sound Health Care System provides tertiary care to veterans throughout the region. Residents will rotate on the General Surgery Service in their intern year and for 2-3 months a year on the Cardiothoracic Surgery Service in their senior years of training. (Located 7.5 miles south of UW Medical Center-Montlake)
- Seattle Children’s Hospital was founded over 100 years ago and serves families across the WWAMI region regardless of their ability to pay. Residents will rotate on the General Pediatric Surgery Service in their PGY 1 and PGY 3 years and will have the option of rotating on the Congenital Cardiac Service in their senior years. (Located 2.0 miles west of UW Medical Center-Montlake)
- Harborview Medical Center serves as the only Level 1 trauma center for the entire WWAMI region. Residents will rotate on a myriad of services at this site in the PGY 1-3 years and are exposed to all aspects of trauma, critical care, and vascular surgery. (Located approximately 5 miles south of UW Medical Center-Montlake)
- University of Washington Medical Center–Northwest is a community hospital located in North Seattle. Integrated residents rotate as the senior resident on the General Surgery Service in their PGY 3 year of training. This rotation is designed to allow trainees to hone their laparoscopic and open surgical skills on “bread and butter” general surgery cases as well as learn to be the “chief” of a service. (Located approximately 6 miles north of UW Medical Center-Montlake)
- Kootenai Health is a regional medical referral center, 397 bed hospital in Coeur d’Alene, Idaho. This away, community rotation provides PGY 4 trainees with the kind of experiences CT surgeons will encounter in community practice.
Rotations
The curriculum and rotations of the PGY 1-3 years are focused on building a strong foundation in surgical skills.
Integrated residents will rotate on general surgery, vascular surgery, cardiothoracic surgery (highlighted rotations below), anesthesia, and ECHO services across six sites of training to attain the prerequisite experience in cardiothoracic surgery. These rotations will facilitate the completion of the ABTS Junior Case Requirements.
The PGY 4-6 years make up the core of cardiothoracic surgery training and time is split between the UW Medical Center Thoracic, UW Medical Center Cardiac, VA, and Kootenai Health services. These final three years of training are intensive, and the Integrated resident is fully immersed in cardiothoracic surgery, working alongside the Traditional fellows (one per year) to truly lead the team and drive patient care. On these rotations, trainees will work one-on-one with Cardiac and Thoracic faculty to master all aspects of Cardiac and Thoracic surgery.
Cardiac Surgery
- Coronary Revascularization
- Valvular Heart Disease
- Endocarditis
- Aortic Surgery
- Advanced Heart Failure
- Mechanical Circulatory Support (MCS)/ECLS
- Cardiac Transplantation
- Structural Heart Disease/Transcatheter Valve Replacement
- Adult Congenital Surgery
Thoracic Surgery
- General Thoracic Oncology
- End-stage Lung Disease/Lung Volume Reduction Surgery (LVRS)
- Tracheal Reconstruction
- Esophageal Surgery
- Interventional Bronchoscopy (including Rigid Bronchoscopy)
- Chest Wall Reconstruction
- Mediastinal and Pleural Disease
- VATS and Robotic Surgery
- Lung Transplantation
- Pulmonary Thromboendarterectomy
- Extracorporeal Life Support
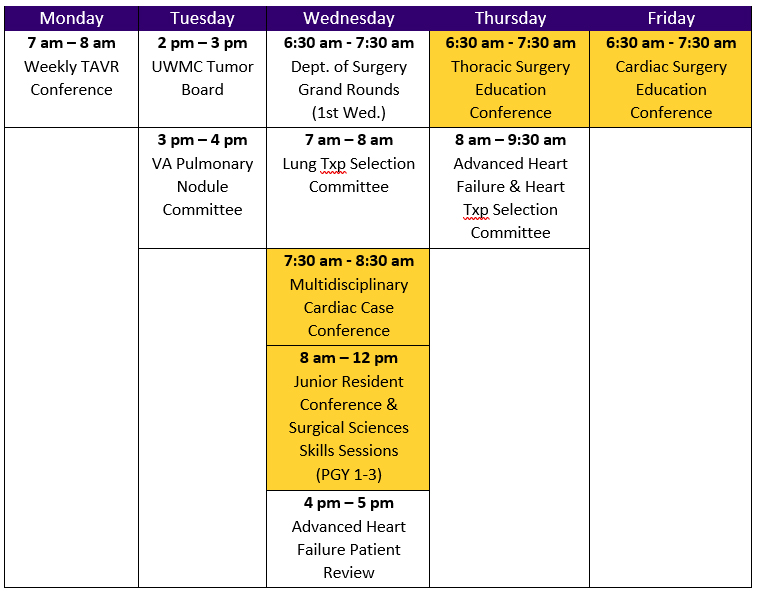
Conferences
Each week residents participate in didactic sessions geared towards establishing and reinforcing a comprehensive understanding of cardiothoracic surgery. The weekly Thoracic Surgery and Cardiac Surgery Education Conferences follow the Society of Thoracic Surgeons’ thoracic surgery curriculum, which UW faculty and residents played a key role in helping to establish. Junior Resident Conference (JRC) occurs every first, third, and fifth Wednesday of the month. This conference is designed to give junior residents a primer in basic cardiothoracic surgery skills and knowledge and to create an opportunity for residents to interact with cardiothoracic faculty.
Sample topics include:
- Coronary Physiology
- Congenital Cardiac Anatomy
- Electrophysiology and Pacemakers 101
- ECLS Skills Sessions
- Basic Echocardiography
- Heart Failure for the Cardiothoracic Surgeon
- Cardiopulmonary Bypass
- Management of Acute Aortic Dissections
- Bedside Chest Procedures
- Thoracic Radiology
- Pulmonary Function Testing
- Post-op Care of the Cardiothoracic Surgery Patient
- Surgical Approach to Lung Cancer
- Surgical Approach to Esophageal Cancer
- Management Mediastinal Masses
- Thoracic Analgesia
Cardiothoracic Surgery In-house Bootcamp
This year was the division’s initial in-house bootcamp for our new trainees as well as current trainees at the start of the academic year. Topis included; ICU management of the post-op cardiac surgery patient; Introduction to the CBP circuit; Bronchoscopy- Flexible and Rigid / Awake Bronch / stenting/ dilation; MCS – ECMO; VAD management and training; Cannulation, CABG, and AVR simulation.
Consistent with Coalition for Physician Accountability recommendations, all interviews will be held virtually via Zoom for the 2022 recruitment cycle.
Recruitment & Selection
The Division of Cardiothoracic Surgery at the University of Washington is a participating member of the National Resident Matching Program (NRMP) and only accepts applications through the Electronic Residency Application Service (ERAS). Paper applications will not be accepted.
Each year the Division of Cardiothoracic Surgery offers 24 interview spots to fill 1 open categorical 1-6 positions.
Applicants must be a graduate of a US or Canadian medical school accredited by the Liaison Committee on Medical Education (LCME), a graduate of a US college of osteopathic medicine accredited by the American Osteopathic Association (AOA), or an International Medical Graduate that fits the criteria below. Canadian applicants should contact the Canadian Residents Matching Service.
Eligible applicants will be considered based on their individual preparedness, ability, aptitude, academic credentials, communication skills, and personal qualities such as motivation and integrity. For Program Leadership and Cardiothoracic Surgery faculty to effectively review applications and select candidates for interviews, in addition to the ERAS application the following items are required:
- Completion of USMLE Step 1 and Step 2 CK exams
- At least three letters of recommendation
The NRMP program code is 1918461C0.
Application Process & Dates
While the Division of Cardiothoracic Surgery will accept applications on a rolling basis throughout the recruitment season, priority will be given to applications received by Wednesday, September 25, 2024. The UW will be following the TSDA guidelines for the Universal Offer Date and will send out the first round of interview invitations by the close of business on Tuesday, October 22, 2024. Applicants will have 48 hours to review their interview schedule and should send their acceptance or declination of an interview by Thursday, October 24, 2024 at 9pm PST. Interviews will be scheduled on Monday, November 4th. We will be offering 24 interview spots, over two interview days, for one categorical position.
We are also using TSDA Program Signaling to better understand which applicants are most interested in the University of Washington. We understand that applicants will NOT signal their home program or programs where they completed a visiting elective.
Interview Dates for AY25:
- December 6, 2024
- January 10, 2025
We will have in-person interviews this year.
Interview Day Process
Overview of Interview Day:
- Program Overview Presentation
- Coffee with Current Residents
- Meeting with Department Chair
- Interviews with Cardiothoracic Surgery Faculty and Chief Residents
To learn more about working at the University of Washington and living in Seattle, please take a look at our social media accounts!
Instagram: @uwctsurgeryresidents
Twitter: @UWCTSurgRes
If you have any questions or would like additional information, please contact:
ctrespa@uw.edu
International Medical Graduates
The Cardiothoracic Surgery – Integrated Program welcomes applications from International Medical Graduates in the following situations:
- If an applicant is a graduate of a medical school outside the United States and Canada who has received a currently valid certificate from the Educational Commission for Foreign Medical Graduates (ECFMG) prior to appointment, or a full and unrestricted license to practice medicine in a US licensing jurisdiction in which they are training.
- If an applicant is a graduate of a medical school outside the US who has completed a Fifth Pathway program provided by an LCME-accredited medical school.
Students and graduates of foreign medical schools should view our Certificate Program for International Physicians. This is a pre-requisite for foreign medical school graduates who seek residency positions in our program.
Virtual Q&A Sessions
TBA
Mentorship
All incoming Integrated Residents are matched with a Cardiothoracic Surgery faculty mentor as interns. Trainees will meet with their mentor on a semi-annual basis to discuss progress and goals.
Additionally, residents meet with the Program Director a minimum of twice a year for reviews.
Leadership
Trainees at the UW have many local and national leadership opportunities.
Past trainees have served in leadership positions for many organizations including:
- Department of Surgery Cardiothoracic Surgery Interest Group
- Department of Surgery Women’s Council
- Department of Surgery Diversity Council
- Department of Surgery Wellness Committee
- UWHA House Staff Association
- Washington State Medical Association, Resident and Fellow Section
- Society for Black Academic Surgeons
- Society of Thoracic Surgeons
- TSRA Executive Committee
- AATS Resident Representative to the ORR/AAMC
The PGY 6 Integrated resident also holds the position of Chief Resident. Together with the senior fellow from they are responsible for managing the weekly Thoracic and Cardiac Education Conference schedules, monthly call schedule, and day-to-day management of the Cardiac and Thoracic Surgery services. The Chief Residents receive a monthly stipend in addition to their base salary.
Research
While residents are invited and encouraged to participate in scholarly activity such as writing manuscripts and books chapters or giving presentations throughout their training, the Cardiothoracic Surgery Integrated Residency does not require trainees to take formal time out for research. However, there are still numerous opportunities for involvement in all aspects of research including clinical outcomes, quality improvement, and work with local and national clinical databases.
Applicants and residents interested in taking additional time out of clinical training for research are encouraged to speak with the Program Director early on in their training.
Training Tracks
The Cardiothoracic Surgery Integrated Residency is designed to provide residents with focused, hands-on experience and is divided equally between Cardiac and Thoracic surgery. While residents are welcome to choose any area of specialty, there are no pre-designated cardiac or thoracic tracks.
The Integrated Program at the University of Washington is truly unique because of the nearly equal division between cardiac and thoracic surgical training. Regardless of a resident’s chosen area of specialty, all graduates of the program are trained to be competent, well-rounded surgeons in both general thoracic and general cardiac surgery.
Educational & Research Conferences
Division of Cardiothoracic Surgery Annual Visiting Professor
Each spring the Division of Cardiothoracic Surgery hosts its annual Visiting Professor Lectureship. This event brings leaders in the fields of Cardiac, Thoracic, and Congenital Surgery from all over the country to Seattle. Each year this event is split into two parts – in the morning residents deliver case presentations and, in the afternoon, the Visiting Professor delivers a keynote speech. The day of academia is followed by a reception and dinner for residents, faculty, and the honored guest.
Past Visiting Professors have included:
- Sean Grondin (Department Head, Surgery; University of Calgary)
- Joseph Dearani (Chair, Cardiovascular Surgery; Mayo Clinic)
- Michael Mack (Medical Director of Cardiothoracic Surgery; Baylor Scott & White Health & Chair; BSW The Heart Hospital – Plano Research Center)
- Keith Naunheim (Director, Cardiothoracic Surgery; Saint Louis University)
- Frank Hanley (Chief, Pediatric Cardiac Surgery; Stanford University)
- Carmelo Milano, (Chief and Professor, Division of Cardiothoracic Surgery, Joseph W. and Dorothy W. Beard Distinguished Professor of Surgery: Duke University)
Harkins Symposium and Strauss Lecture
Named in honor of the Department of Surgery’s first Chairman and an esteemed University of Washington alumnus respectively, the Harkins Symposium and Strauss Lecture is a day of scholarship held each fall in which faculty across the Department of Surgery present on the insightful, cutting-edge research currently being done at the University of Washington. The Strauss Lecture is delivered each year by an invited professor who is a leader in the field of surgery.
Past speakers have included:
- Valarie W. Rusch (Vice Chair for Clinical Research, Department of Surgery; Memorial Sloan Kettering)
- Jonathan Woodson (Director, Institute for Health System Innovation & Policy; Boston University)
- Andrea L. Pusic (Chief, Plastic and Reconstructive Surgery; Brigham and Women’s Hospital)
- Robert S.D. Higgens (Director; Department of Surgery; Johns Hopkins University)
- Thomas M. Krummel (Emile Holman Professor Emeritus (Active), Co-Director, Stanford Byers Center for Biodesign Program, & Director, Surgical Innovation Program; Stanford University)
Dr. Steven C. Stain, (Department of Surgery Chair at Lahey Hospital and Medical Center, and Department of Surgery Professor at Tufts University School of Medicine)
Resident Research Day and Schilling Lecture
Dr. John Schilling was the third Chairman of the Department of Surgery and is remembered as laying the groundwork that made the Department what it is today. In his relatively short eight-year tenure as Chair, Dr Schilling recruited 41 faculty and graduated 40 chief residents. Each year in his honor, the Department of Surgery hosts the Resident Research Day and Schilling Lecture.
Over the course of the day, residents from the five departmental divisions (General Surgery, Cardiothoracic Surgery, Transplant Surgery, Vascular Surgery, and Plastic Surgery) are invited to present their research to faculty mentors and peers. The Schilling Lecture is delivered by an invited professor who shares Dr. Schilling’s devotion to patient care, teaching, and research.
Past lecturers include:
- Mary Hawn (Chair, Department of Surgery; Stanford University)
- Caprice C. Greenberg (Morgridge Distinguished Chair in Health Services Research, Surgical Oncology; University of Wisconsin)
- Diana Farmer (Chair, Department of Surgery; UC Davis)
- Melina Kibbe (Chair, Department of Surgery, University of North Carolina)
- Walter Pories (Founding Chair of the Department of Surgery; East Carolina University)
Department of Surgery Education Seminar
Surgical education is at the heart of the Department of Surgery’s mission. Every June, the entire Department of Surgery gathers to discuss a topic within surgical education with the goal of improving the training of our residents as well as improving the culture of the Department. Both Faculty and trainees are invited to present and lead the discussion.
Past topics have included:
- Strategies and Best Practices for Surgeon-Patient Interpersonal Communication
- Autonomy in Surgical Education
- Wellness Education in Surgery
- Leadership Skills and Development
Graduates
 Kathleen S. Berfield, MD |
 Edo Bedzra, MD, MBA |
 Christopher Ryan Burke, MD |
 Eric Howell, MD |
 Swaroop Bommareddi, MD |
 Tori Lennox, MD |
Salary and Benefits
The University of Washington offers residents a wide range of benefits as part of their total compensation package. These include:
- Four weeks paid vacation
- Medical, dental, and life insurance
- Retirement plans
- Coverage of certification costs
- Annual professional development fund
Since 2016 residents at the University of Washington have been represented by the University of Washington Housestaff Association (UWHA). As such the benefits and compensation for all trainees in the Cardiothoracic Surgery – Integrated program are in compliance with the Collective Bargaining Agreement (CBA).
For more information on the benefits offered to residents and a copy of the current stipend schedule, visit the UW GME website for prospective residents and fellows.
In addition to the benefits offered in the CBA, the Cardiothoracic Surgery – Integrated program provides its residents with:
- Pair of 2.5x loupes in PGY 2 year
- Pair of 3.5x loupes in PGY 4 year
- Annual STS candidate membership
- Support for conference attendance
Seattle offers its residents unrivaled access to both a vibrant, culturally diverse urban center and the storied outdoor recreation of the Pacific Northwest. When asked about the reasons that they love to live here, our faculty and trainees often cite the proximity of culture and recreation in Seattle – for instance, the opportunity to hike on the Olympic Peninsula on Saturday morning and eat at a James Beard award-winning restaurant that night.
Where do residents live?
Living in Seattle offers access to an enviable array of amenities including:
- Three ski resorts within two hours of the city
- Local MLB, NFL, MLS, WNBA, NHL teams
- 60+ breweries operating within city limits
- Thriving museum culture (including art, history, cultural, and children’s museums)
- Robust theater and music scene (ranging from Seattle Symphony to Broadway shows to live concerts)
- Seattle International Film Festival
Many neighborhoods throughout the city are easily accessible to our six primary sites of practice. In a recent survey, trainees in the Department of Surgery identified where they live. See the map below for details.
Most residents rent while in a training program and 97% pay $2500 or less per month.
- 61% live with a partner
- 26% have a platonic roommate
- 11% have children
- 42% have pets
- 65% have house plants
Will I need a car?
While many trainees in the Department of Surgery live in neighborhoods that are easily walkable to our sites of practice and Seattle is regularly ranked as one of the most bike and public transit friendly cities in the country, most of our residents own cars and drive to work each day.
This decision is often based on convenience due to the dynamic work schedule, but also affords residents the opportunity to easily explore the Pacific Northwest on their days off.
Some great examples of day trips include:
- Mount Rainier
- San Juan Islands
- Washington Wine Country
- Olympic National Forest
- Portland, OR
While many trainees in the Department of Surgery live in neighborhoods that are easily walkable to our sites of practice and Seattle is regularly ranked as one of the most bike and public transit friendly cities in the country, most of our residents own cars and drive to work each day.
This decision is often based on convenience due to the dynamic work schedule, but also affords residents the opportunity to easily explore the Pacific Northwest on their days off.
Some great examples of day trips include:
- Mount Rainier
- San Juan Islands
- Washington Wine Country
- Olympic National Forest
- Portland, OR
Community Life in our Department
In addition to holding regular education events throughout the year, the Department of Surgery also works to foster collegiality and friendship among its faculty and trainees with more social events. These include:
- Resident Ski Day
- Resident Happy Hours
- Department of Surgery Annual Picnic
- Department of Surgery Holiday Party
- Department of Surgery Oyster Fry
The Division of Cardiothoracic Surgery also hosts several events throughout the year including:
- Annual Residency Summer Barbeque
- Division Holiday Party
- Division of Cardiothoracic Surgery Graduation Ceremony
The 4/3 Cardiothoracic Surgery Residency Program is designed for general surgery residents that are identified early on in their training as having an interest in pursuing a career in cardiothoracic surgery. To be eligible to apply for this program, candidates must be a current University of Washington general surgery categorical resident in good standing.
- If you are a UW trainee interested in the 4/3 program, please contact ctrespa@uw.edufor more information.
- For questions, please contact our Program Administrator:
- ctrespa@uw.edu
The 4/3 Cardiothoracic Surgery Residency Program is designed for general surgery residents that are identified early on in their training as having an interest in pursuing a career in cardiothoracic surgery. To be eligible to apply for this program, candidates must be a current University of Washington general surgery categorical resident in good standing.
If you are a UW trainee interested in the 4/3 program, please contact ctrespa@uw.edu for more information.
For questions, please contact our Program Administrator:
ctrespa@uw.edu