Cardiothoracic Surgery-Traditional
Cardiothoracic Surgery-Traditional
About the Program
The Cardiothoracic Surgery Traditional Fellowship program is dedicated to producing balanced, well-qualified cardiothoracic surgeons prepared to serve the community through careers in either private practice or academia. With dedicated faculty based at Seattle’s premier medical facilities, the program has been carefully designed to balance training in cardiovascular and thoracic surgery.
This two-year fellowship is designed to provide trainees with focused, hands on experience divided equally between cardiac and thoracic surgery. While fellows are welcome to choose an area of specialty, there are no pre-designated cardiac or thoracic tracks.
Fellows rotate on cardiothoracic surgery clinical services at two main sites of practice with senior residents in the Cardiothoracic Surgery Integrated Residency program. Throughout these two years of training, fellows will gain requisite experience in general thoracic, cardiac, congenital cardiac, and foregut surgery as well as end-stage heart and lung disease, including mechanical circulatory support and heart and lung transplantation.
Quick Facts
- Faculty have served as leaders of STS, ABS, ABTS, WTSA, TSDA, ACS, JCTSE, ISHLT, ELSO, and the ACGME Thoracic Surgery Residency Review Committee
- Division has completed 1000+ lung transplants and 900+ heart transplants
- Average case numbers at graduation: 811 total cases
Program Leadership
Program Director
Associate Professor, Division of Cardiothoracic Surgery
Chief of Thoracic Surgery VA Puget Sound HCS
Associate Program Director
Associate Professor, Division of Cardiothoracic Surgery
Clinical Experience
Cardiothoracic Surgery fellows at the University of Washington receive an unrivaled clinical education. Training alongside nationally and internationally recognized faculty, fellows have a robust operative experience in every subspecialty of cardiothoracic surgery from “bread and butter” cases” like CABGs and lobectomies to more complex cases like hybrid aortic aneurysm repair and pulmonary thromboendarterectomy.
What makes the fellowship program at the University of Washington unique is that it is one of the few programs in the country that trains you to be a true Cardiothoracic surgeon. Graduates are equipped to handle the full spectrum of cardiac and thoracic surgical disease. Additionally, as the tertiary and quaternary referral center for the WWAMI region, we care for a diverse patient population, which equates to a robust clinical experience.
Fellows primarily rotate on three services – UW Medical Center Thoracic Surgery, UW Medical Center Cardiac Surgery, and VA Puget Sound Healthcare System Cardiothoracic Surgery – and are integral members of the surgical team both in and out of the OR. Our fellows work alongside a dedicated APPS in the ICU, Acute Care floor and OR as well as Integrated residents and oversee all aspects of perioperative care from the initial clinic visit until discharge, giving them a well-rounded clinical experience.
Training Sites
Traditional Cardiothoracic Fellows will rotate at three sites throughout their training.
- The University of Washington Medical Center – Montlake is a tertiary and quaternary care referral site for the WWAMI region and serves as the primary training site for the fellowship. Fellows will split their time at this site between the Cardiac and Thoracic Services.
- The VA Puget Sound Health Care System provides tertiary care to veterans throughout the region. Fellows will rotate for 2-3 months a year on the Cardiothoracic Surgery Service. (Located 7.5 miles south of UW Medical Center-Montlake)
- Seattle Children’s Hospital was founded over 100 years ago and serves families across the WWAMI region regardless of their ability to pay. Fellows interested in Congenital Cardiac surgery will have the option of rotating on the Congenital Cardiac Service. (Located 2.0 miles west of UW Medical Center-Montlake)
Rotations
Training is split between the UW Medical Center Thoracic, UW Medical Center Cardiac, and VA Puget Sound Health Care System services. These two years of training are intensive, and fellows are fully immersed in cardiothoracic surgery, working alongside the senior Integrated residents to truly lead the team and drive patient care.
On these rotations, trainees will work one-on-one with Cardiac and Thoracic faculty to master all aspects of Cardiac and Thoracic surgery.
Cardiac Surgery
- Coronary Revascularization
- Valvular Heart Disease
- Aortic Surgery
- Endocarditis
- Advanced Heart Failure
- Mechanical Circulatory Support (MCS)/ECLS
- Cardiac Transplantation
- Structural Heart Disease/Transcatheter Valve Replacement
- Adult Congenital Surgery
Thoracic Surgery
- General Thoracic Oncology
- End-stage Lung Disease/Lung Volume Reduction Surgery (LVRS)
- Tracheal Reconstruction
- Esophageal Surgery
- Interventional Bronchoscopy (including Rigid Bronchoscopy)
- Chest Wall Reconstruction
- Mediastinal and Pleural Disease
- VATS and Robotic Surgery
- Lung Transplantation/ ECLS
- Pulmonary Thromboendarterectomy
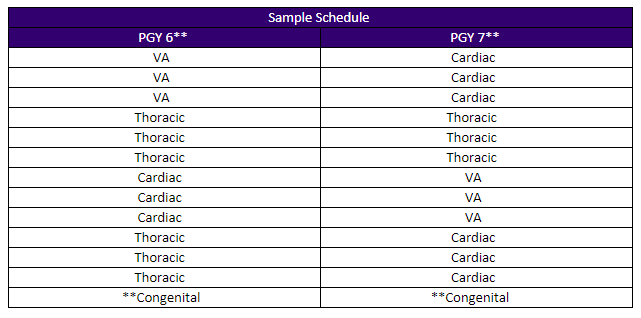
*Please note: This is a sample schedule indicative of the average rotation schedule for a Traditional Fellow. ** In the PGY 6 or 7 years of training there is an option to rotate on the Congenital Cardiac Service at Seattle Children’s Hospital.
Conferences
Each week fellows participate in didactic sessions geared towards establishing and reinforcing a comprehensive understanding of cardiothoracic surgery.
The weekly Thoracic Surgery and Cardiac Surgery Education Conferences follow the Society of Thoracic Surgeons’ thoracic surgery curriculum, which UW faculty and trainees played a key role in helping to establish.
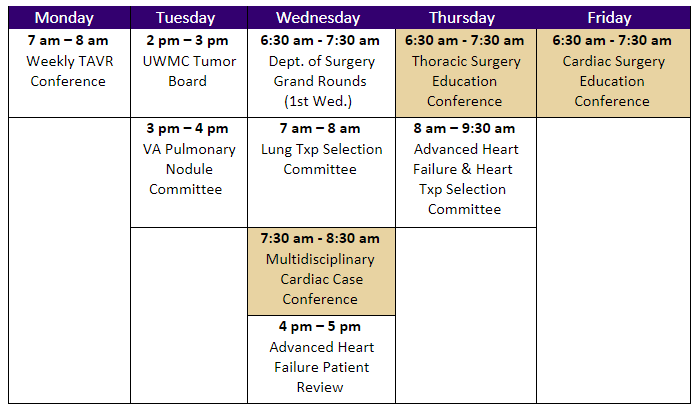
*Highlighted conferences are mandatory Cardiothoracic Surgery resident conferences.
Simulation Training
In their PGY 6 year Traditional Fellows participate in a 35-week simulation training at the WWAMI Institute for Simulation in Healthcare (WISH) that will cover three basic cardiac surgery procedures and three critical intraoperative adverse events:
- Cardiopulmonary bypass (CPB)
- Coronary artery bypass surgery (CABG)
- Aortic valve replacement (AVR)
- Massive intraoperative air embolism (MAE)
- Acute intraoperative aortic dissection (AIAD)
- Sudden perioperative deterioration of cardiac function (SDCF)
Simulation training is led weekly by a Cardiothoracic Surgery faculty member, with participation from members of the nursing, perfusion, and anesthesia teams as needed. Completion of this curriculum meets the simulation training requirements for ABTS board eligibility.